
Nicholas Peat
08 December 2023
The intricate ecosystem within our digestive system plays a pivotal role in shaping our overall health and well-being. When we think of the gut, we often think about digesting food. But inside, it is a complex network of microorganisms that influences various aspects of our physiology, ranging from immune function to mental health.
When the delicate balance of the gut is disrupted, it can lead to a cascade of health issues. From digestive discomfort to more severe conditions, such as Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD), the repercussions of compromised gut health extend far beyond the intestines. Far beyond what some people may see as ‘stomach ache’ or ‘bloating.’ Indeed, the impact is systemic, affecting daily lives, including energy levels, cognitive function, and even emotional resilience.
Understanding the significance of maintaining a healthy gut is paramount. It empowers you to make informed choices that can positively shape your overall quality of life. So, let’s dive into the basics of gut health and why we’re so passionate about it.
Understanding the gut
What seems like a simple digestive system is actually complex and incredible, but let’s start with the basics. The gut's primary role is to digest and absorb nutrients from the food we consume, beginning with mechanical and chemical processes in the mouth and continuing through the stomach and small intestine. This digestive process ensures the body receives essential proteins, fats, and carbohydrates for energy and overall health.
Additionally, the gut acts as a crucial barrier against harmful microorganisms, supporting the immune system. The gut microbiome, a diverse community of microorganisms within the digestive tract, further contributes to health by synthesising vitamins and aiding in the fermentation of undigested carbohydrates. In essence, the gut plays a central role in nutrient absorption, immune function, and the dynamic interplay with the microbiome, all vital for maintaining overall wellbeing.
The guts command centre
The enteric nervous system (ENS), often referred to as the "second brain" or the gut's command centre, is a complex network of neurons embedded in the lining of the gastrointestinal tract. This intricate system operates independently, communicating with the central nervous system but capable of functioning autonomously. Comprising over 100 million neurons, the ENS regulates essential gut functions, including peristalsis, secretion, and blood flow.
Beyond its role in digestion, the ENS is increasingly recognised for its influence on mood, cognitive disorders, and overall well-being. In fact, there’s lots of new research exploring the relationship between the gut, the brain, and the microbiota (microbes in our body) in causing neurodegenerative diseases. It particularly focuses on how problems in the gut, like issues with the microbes and inflammation, might be connected to Parkinson's Disease or Alzheimer’s. The hope is that by understanding and fixing these gut issues, scientists could develop new ways to diagnose these types of conditions early and develop treatments to slow them down.
This is just the tip of the iceberg regarding current gut research. Scientists continue to uncover the multifaceted role of the ENS, highlighting its significance not only in digestive processes but also in the broader context of human physiology and the intricate interplay between the gut and the brain. What we do know for sure is that looking after your gut health is paramount to looking after your overall health and wellbeing.
The gut-brain connection
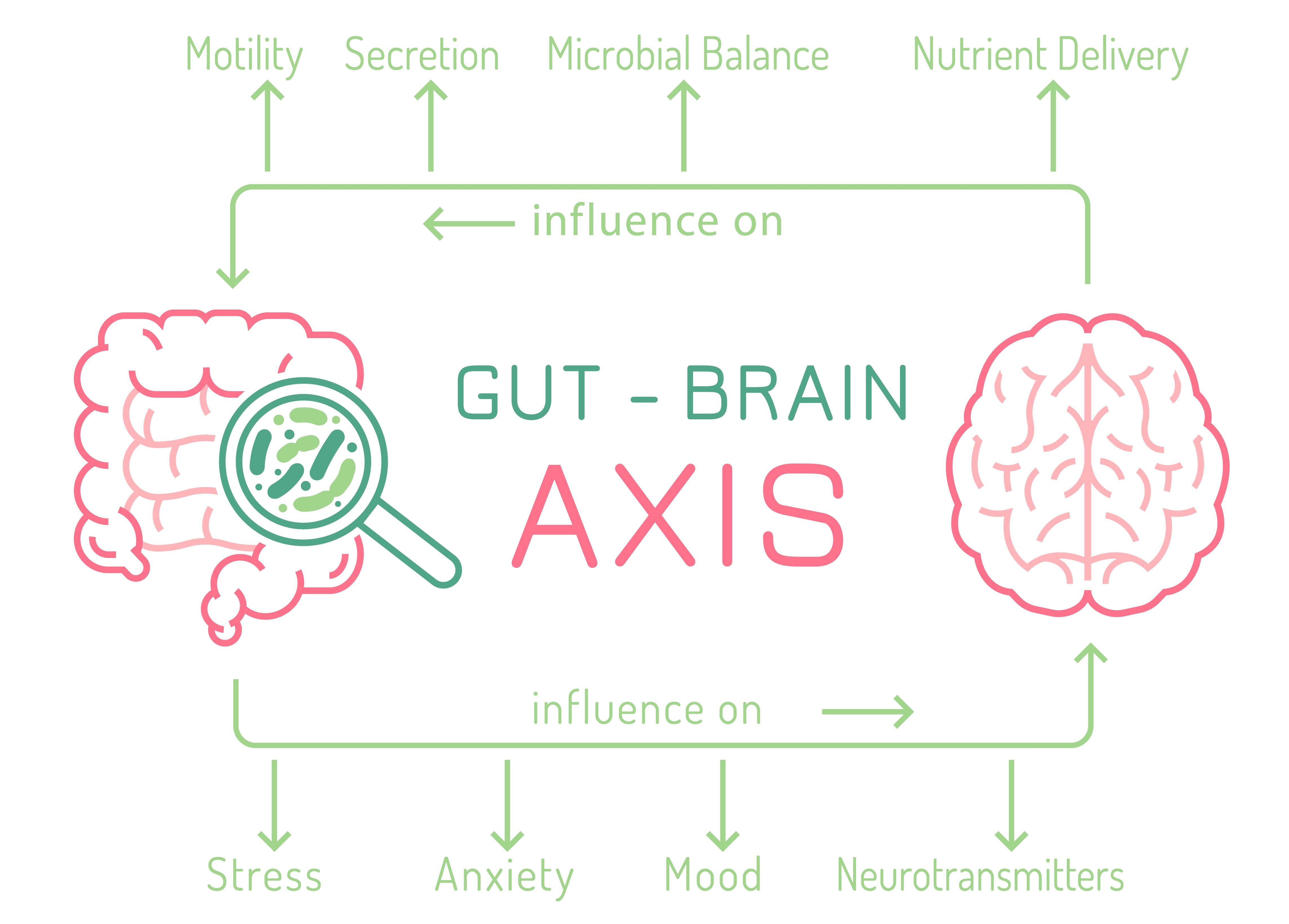
The gut-brain axis is a bidirectional communication system that connects the central nervous system (brain and spinal cord) with the ENS of the gastrointestinal tract. This intricate network enables constant communication between the gut and the brain, influencing various physiological and behavioural processes. Signals travel along this axis through neural pathways, immune system molecules, and metabolic products.
The gut-brain axis plays a crucial role in regulating digestive functions, nutrient absorption, and gut motility. Moreover, emerging research has highlighted its impact on mental health, mood, and cognitive function. Factors such as the gut microbiome, neurotransmitters, and hormones contribute to this communication, emphasising the interconnectedness of gut health and brain function.
Disruptions in the gut-brain axis have been associated with conditions like IBS, highlighting, as we have mentioned, the significance of this complex interplay in maintaining overall health and well-being. So, let’s take a look at IBS and IBD in a bit closer detail.
Irritable Bowel Syndrome
The National Institute for Health and Care Excellence states around 10-20% of the UK population has IBS, although they suggest the true prevalence is likely higher as many people with IBS symptoms do not seek medical advice. It’s a disorder of the gut-brain axis showcasing the powerful connection between the gastrointestinal system and the brain. IBS disrupts the normal functioning of the gut, leading to a range of symptoms, such as abdominal pain, bloating, and irregular bowel habits. The gut-brain axis plays a crucial role in regulating these digestive processes, and when it falters, it can result in debilitating symptoms for individuals with IBS.
The impact of IBS extends beyond the physical realm, influencing overall well-being and quality of life. The need to navigate potential triggers and the fear of symptom flare-ups can influence social activities, work commitments, and overall quality of life. Research from the United States identifies that people with IBS miss an average of 13.4 days of work or school yearly, compared to 4.9 days for those without IBS. Another survey found that 24% of respondents missed work in the last week due to IBS symptoms, and 87% experienced reduced productivity at work during the same period. Having to live with IBS symptoms can lead to people experiencing heightened stress, anxiety, and a sense of unpredictability.
Stress and IBS are intrinsically linked. Whether emotional or psychological, stress can trigger or exacerbate IBS symptoms. On one hand, stress can directly affect gut motility, leading to changes in bowel habits and increased sensitivity to pain. On the other hand, the gut, particularly the intestines, has a rich network of nerves that are highly responsive to stress signals. This bidirectional communication can create a vicious cycle where stress worsens IBS symptoms, and the discomfort caused by IBS, in turn, contributes to increased stress levels. This is something our co-founder at Uniquely Created U (USU) knows all too well.
Vanessa Peat, Co-Founder of UCU, Performance Nutritionist, and Registered Associate Nutritionist, suffered from stress-related IBS as a neurodiverse individual while in academia. It’s one of the reasons behind creating UCU and developing effective IBS management through a truly personalised approach. Each individual’s experience with IBS is unique, demanding a tailored plan that addresses not just dietary needs but also lifestyle adjustments and psychological support. Cognitive behavioural therapy and gut-directed hypnotherapy have the most extensive evidence base for helping to manage IBS. Similarly, a completely individualised approach is also required to manage other gut conditions like IBD.

Inflammatory Bowel Disease
IBD is a term used to describe a group of chronic disorders characterised by inflammation of the gastrointestinal (GI) tract. The two primary types of IBD are Crohn's disease and ulcerative colitis.
In Crohn's disease, inflammation can occur anywhere along the GI tract, from the mouth to the anus, and it often involves all layers of the intestinal wall. On the other hand, ulcerative colitis specifically affects the colon and rectum, causing inflammation and ulcers in the lining of the large intestine. Crohn’s and Colitis UK advise that one in every 123 people has a diagnosis of IBD. This means over 500,000 people in the UK are currently living with this condition.
Unlike IBS, which is a functional disorder, IBD involves inflammation and structural damage to the digestive tract. IBD is a chronic condition with periods of flare-ups and remission, and its exact cause is not fully understood, involving a combination of genetic, environmental, and immune system factors.
Symptoms of IBD encompass urgent and frequent diarrhoea, sometimes accompanied by blood, along with abdominal pain, fatigue, and weight loss. These symptoms bring about anxiety and depression, resulting in absenteeism from school or work, withdrawal from social connections, and difficulty performing everyday activities like shopping and exercising. Physical complications can also become severe for some, leading to surgical intervention. These complications were experienced by the other co-founder of UCU - Dr Nicholas Peat.
One night, it all changed for Nicholas. He collapsed, feeling an odd sensation in his stomach that quickly turned into excruciating pain. Being a doctor, he knew it wasn't a minor issue, and he suspected peritonitis, inflammation inside the sterile part of the abdomen. Driving to the hospital was agony with every bump, and upon arrival, he vomited on a colleague's shoes. An x-ray confirmed a bowel perforation. He underwent surgery where 30cm of his small intestine had to be removed. In the aftermath, he was diagnosed with severe Crohn's disease, leading to a period of fear and uncertainty about what lay ahead.
In Nicholas's journey, he, like Vanessa, discovered that stress played a role in triggering his health challenges, especially his IBD. Studies reveal that stress can have a detrimental effect on people diagnosed with IBD. Scientists advocate that healthcare professionals should actively educate people with IBS about the advantages of stress reduction. Recognising this, Nicholas dove into the world of stress management techniques, determined to regain control over his well-being.
Simultaneously, he revamped his diet to better suit his unique needs and embraced a new fitness routine. We won’t get into specific diets in this article, but addressing diet is an essential part of managing gut disorders. For example, recent studies suggest a low FODMAP diet can benefit individuals with ulcerative colitis and Crohn's disease. One research study demonstrated improvement in IBD-related symptoms like abdominal pain, bloating, and diarrhoea in 72% of patients with Crohn’s disease and 78% of patients with ulcerative colitis without active inflammation following a low FODMAP diet. But more on that another time.
The combination of Nicholas’s efforts worked wonders, significantly easing his symptoms and granting him a vastly improved quality of life. What sets Nicholas's story apart is his remarkable fortune—instead of resorting to steroids or conventional pharmaceuticals, he achieved complete and sustained remission through substantial changes in his diet and lifestyle.
Creating Uniquely Created U
Now you’ve heard just a small part of Nicholas and Vanessa’s stories, it might make sense why they created Uniquely Created U. UCU blends their personal experiences with clinical expertise to address the challenges posed by gut disorders like IBS and IBD. These conditions can significantly impact your life, demanding a holistic approach for effective management. When navigating the complexities of gut disorders, taking charge of the situation is not only possible but essential for a fulfilling life.
Gut health issues affect millions globally, and understanding the gut and seeking the right support is crucial for symptom control and overall well-being. Armed with knowledge and embracing personalised lifestyle modifications, people facing inflammatory bowel or related diseases can not only cope but thrive in the face of these challenges.
